Using an Advisory Council
A CNO Approach to Engaging Front-line Nursing Staff
As nurse leaders, we are all concerned with the impact of the nursing shortage. As the CNO of a large academic hospital in Atlanta, I am very concerned about the future impact it will have on our hospital and our state. According to the National Center for Health Workforce Analysis, by 2030 Georgia is on pace to have the sixth-highest gap nationwide between supply and demand for nurses. While several factors are contributing to this shortage, it is critical to explore and implement strategies to retain nurses in the profession and at the bedside. As I collaborate with other nurse leaders throughout the nation, I have become aware of an ongoing exploration of innovative ideas to enhance nurse engagement and nurse retention. An extensive body of research utilizing the Kanter Work Empowerment Theory demonstrates a positive correlation between nurse empowerment, engagement and retention. According to Kanter (1993) when employees have access to information, support, resources, development opportunities, formal and informal power, they are empowered to accomplish meaningful work. Reading the questions in your employee annual surveys, you will find the questions seeking to illicit employee perceptions of the access to information, support, resources, development opportunities and power at your organization.
As Grady leaders reviewed our annual employee survey, we saw opportunities to improve our nurses’ perception of empowerment, support and access to information. We also were struggling with high turnover and low retention. After examination of our professional practice councils—and based on recommendations for our Magnet consultant—we decided to implement unit-based councils and restructure our professional practice councils. The goal of the restructure was to coach and support the clinical staff in leading the councils and active decision-making. Through the unit-based councils, department councils and professional practice councils, we wanted to put in place ongoing bi-directional communication to ensure the clinical staff were informed and aware of the councils’ many projects. While this did improve the knowledge of a subset of the front-line staff, leaders at Grady Health System were not happy with the level of engagement and realized more work needed to be done.
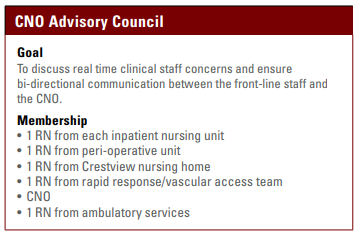
While at the 2017 Magnet conference, I attended a leadership session titled “Increasing Clinical Nurse Engagement through a CNO Partnership with Leaders at the Bedside.” The session discussed how the CNO developed a “cabinet” of clinical nurses from across the organization to increase bi-directional communication and collaboration between the CNO and front-line staff. This innovative idea could improve nurse engagement through real-time, ongoing communication. Upon returning to Atlanta, we considered how we could replicate a CNO partnership with front-line staff at Grady. We received such positive feedback from the CNO nursing forums that we knew this was something we needed. We landed on the CNO Advisory Council. The council would meet once a month for two hours. Nurse leaders were asked to collaborate with their unit-based councils and select a clinical nurse who was committed to Grady’s mission and vision to represent their unit at the CNO Advisory Council.
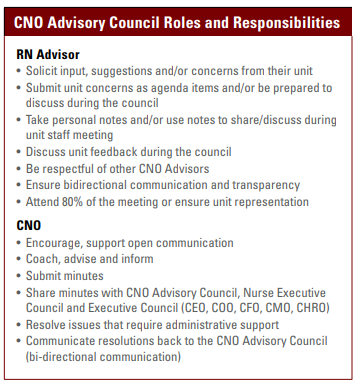
CNO Advisory Council
Our inaugural CNO Advisory Council kickoff was November 16, 2017. The meeting began with roundtable introductions, the why (we need a CNO Advisory Council), goals of the council and roles and responsibilities of the council members. The group was diverse and its members’ experience ranged from two years to over fifteen years, with ages ranging from 24 to late 40s, with the majority of members in their mid-30s. The group reviewed and discussed the pre-reading assignment and spent time discussing their roles and getting comfortable with each other. Since this was the first meeting, and not everyone was aware of what they were supposed to do, I provided examples of concerns from the annual employee survey. Members were requested to solicit concerns from their peers.
Change in uniform
In February 2018, I added uniforms to the agenda and asked the advisors to come prepared to discuss concerns regarding white uniforms. The nurses at Grady wear white; during my time at Grady, I have been asked on different occasions if the nurses can wear non-white. The advisors did a phenomenal job eliciting information from their units; they were very well prepared to discuss the positives and negatives about the work uniforms. Based on the feedback, it was apparent it was time for change; however, a subset of nurses preferred to wear white.
The council agreed the next step would involve informally surveying the unit staff on the following:
1. Would you like to wear all white?
2. Would you like the option of wearing both white (all) and the option of wearing non-white (all)?
3. If you had the option of wearing non-white, please select two to three colors.
Each advisor submitted the results of the informal survey, and the color selections. After receiving the color recommendation from each unit, a formal survey was sent to over 1,500 nurses.
1. Would you like to wear all white?
2. Would you like the option of wearing either white (all) and the option of wearing non-white (all)?
3. If you had the option of wearing non-white, please select one color.
We had an 80% response rate to the survey in which the nurses wanted the option of wearing either all white or all non-white. The color royal blue received most votes. A couple of departments were not happy with the color selection and wanted a re-vote. This was taken back to the council; it decided the vote was fair and the decision was made. The council also decided on the types and color of the jackets and long-sleeve undershirts that can be worn.
While this may seem like a small change, it illustrates the way the council was able to give a voice to nursing staff.
Moving forward
We celebrated our one year mark in November 2018. We have 22 advisors that represent the majority of units and service lines. The themes of the staff concerns/discussions have included:
1. Nurse engagement/empowerment
2. Employee safety/violence/off-site parking
3. Hospital environment of care
4. Bedside shift report/communication
5. Clinical ladder structure
6. Resources
7. Staffing, time and attendance
The CNO Advisory has been instrumental in:
1. Changing employees ID badges to list first name only for front-line nurses and front-line clinical staff to enhance employee safety
2. Implementing the option of non-white uniforms.
3. Nurse phone selection for Rover implementation
4. Ensuring equality in charge nurse pay
5. Providing recommendations for consistency in bedside shift support
After a year, the CNO Advisory Council has grown in understanding its role and alignment with organizational goals. We do not have data on RN turnover; however, when comparing our 2017 RN engagement survey to 2018 we saw improvement in five of seven Magnet categories. We are not at benchmark with our peer group and more work remains. As noted by one of council member, “I have thoroughly enjoyed serving on the CNO Advisory Council. I enjoy being able to take information back to the NICU. . . I love to tell the staff during our monthly staff meetings, ‘Our CNO wants to hear from you! She is very much interested in what works and what does not work.’ I also tell the staff, ‘She wants to make sure the information is flowing up and down.’ The decisions made in this room must get back to the bedside nurse. We can no longer operate in silos. As a result of the council, I believe the staff feels involved and they know their voices matter. The uniform decision-making process was evidence that they’re being heard.”
References
Kanter, R.M. (1993). Men and women of the corporation. (2nd ed.) New York, NY: Basic Books.
U.S Department of Health and Human Services, Health Resources and Services Administration Bureau of Health Workforce National Center for Health Workforce Analysis. (2017). Supply and demand projections of the nursing workforce: 2014-2030.
About the Author
Jacqueline Herd, DNP, RN, NEA-BC
Executive vice president and chief nursing officer at Grady Health System in Atlanta


