
It Takes a Village
“Coming together is a beginning; keeping together is progress; working together is success.” – Henry Ford
Collaborating to Improve First-Year Nurse Retention
Grady Health System of Atlanta is an 800-bed nationally acclaimed Level l trauma center, a Baby Friendly designation, and has a comprehensive burn center and an advanced comprehensive stroke center. Grady is a pillar in Georgia, renowned for healing the patients with formidable health conditions and caring for the indigent and underserved. The health system is responsible for training most of the practicing physicians in Atlanta. Grady is also a premier employer for graduate millennial nurses seeking a health system to begin and catapult their careers. Grady has a solid culture of serving others, providing the new millennial nurses an opportunity to fulfill their need to do meaningful work. Hundreds of applications for the nurse residency program are submitted annually. Typically, a potential nurse resident is euphoric if scheduled for an interview. They enter the organization victorious, grateful, joyous, eager, engaged and proud to be “Grady nurse.” However, early in 2016 a trend was identified: a substantial number of nurse residents were leaving the health system between six to 12 months of employment. Why the exodus? The organization failed to identify millennials as primary stakeholders and meet their needs. This article will focus on the collaborative leadership and cooperation that resulted in the restructuring and rejuvenation of the nurse residency program which in turn, improved first-year retention.
Stakeholders and Silos
The 2010 Institute of Medicine report The Future of Nursing: Leading Change, Advancing Health highly recommended the use of a transitional program for new nurses entering the workforce. Grady Health System received a grant to implement a nurse residency program. The program’s evidence-based curriculum and tools were used to improve first-year retention. Unfortunately, it was not the primary focus of any stakeholder who interacted with the nurse residents (Figure 1).+

The chief nursing officer discovered alarming data regarding first-year new nurse retention: An approximate retention rate of 55–65% between 2013 and early 2016. Deeper analysis revealed only one department and one nurse residency program coordinator were charged with improving nurse resident retention. Upon further investigation, it was discovered that communication and collaboration was poor between the stakeholders who directly impact first-year nurse resident retention and initial experiences. Clearly, the stake-holders were working in silos with separate goals.
The following provides a glimpse of the primary stakeholders, their goals and the processes in place producing gaps:
Human Resources
The talent acquisition team was primarily responsible for the recruitment and onboarding of the nurse resident. Its primary goal was to hire as many new graduates as possible to meet staffing demands. However, this was done without regard to organizational or clinical fit or alignment to nurse residency program start dates. The team had minimal knowledge of the nurse residency program processes and execution. Communication with the program coordinator was at a minimum and the team often had a poor response time to applicants’ emails and calls regarding changing start dates or their preferences to work in certain clinical areas.
Program Coordinator
The primary goal of the program coordinator was to deliver the nurse residency program’s evidence-based curriculum. This was one job duty among many others. Additionally, the nurse residents were provided with a schedule of classes. Other duties were to promote discussions and act as sounding board, sharing successes, challenges and strategies to survive. The nurse residents were required to produce an evidence-based practice project, but received scant leadership support. The coordinator kept attendance records, but had minimal conversations with unit directors, human resources and advanced clinical nurse educators. Advocating for the nurse resident was not a priority.
Advanced Clinical Nurse Educators
The advanced clinical nurse educator/clinical nurse specialists’ (ACNE/CNEs) primary goal was to meet with the nurse residents to discuss and to distribute an orientation plan and expectations. They sporadically monitored progress and had some or no interaction with preceptors. Nurse residents were assessed the same as experienced nurses during orientation. The ACNE/CNEs rarely communicated issues to program manager.
Unit Director
The primary goal of unit directors was to fill their vacancies. At that time, the directors encouraged an expedited orientation of the nurse resident. Preceptors were assigned who had minimal training and interest. Directors minimally met with nurse residents to identify their needs and were not knowledgeable of the nurse residency program guidelines/expectations. They provided inconsistent support for the nurse residency program and had poor attendance at nurse residency program events.
Department of Nursing Education, Practice and Research
The department was assigned accountability and responsibility for the success of the program. It assigned personnel to implement the program as one of many job duties.
There was little evidence from any of the listed stakeholders to show they had retention in their lists of priorities. The stakeholders and others were brought together to address one collaborative goal: retention of the nurse resident in the first year.
Sharing this goal would require a mutual restructuring on how the stakeholders conducted business. They had to become connected and fluid to meet the needs of the nurses. While the stakeholders were developing strategies to symbiotically retain the nurse resident, other collaborations were in process. The chief nursing officer solidified the cooperation and collaboration among the organization’s executives for the necessary resources needed to support first-year nurse retention and the nurse residency program. It was through this administrative influence that the nurse resident and the nurse residency program gained increased visibility and became a central organization focus.
The nurse resident at first was not recognized as a stakeholder. However, nurse residents’ feedback and input was needed to assure that what was important to them was incorporated into the health system’s strategies and goals.
Nurse Resident Experiences
Nurse residents of today want to be valued, heard and feel recognized for their input. The following experiences were derived from nurse statements in residency sessions.
Nurses were dissatisfied with the interview and hiring process, with poor communication at every step in the process. Some said they had inaccurate communication about where they would be working, with some changing nursing units immediately after arrival at the health system. Others said they didn’t have the opportunity to sign a contract until after hire.
They expressed coming into non-welcoming clinical environments, with disorganized unit orientation, lack of management support and visibility and working months before beginning the nurse residency program. By that time, they were unsure of program’s value.
Some said they were paired with unengaged/harsh preceptors. New nurses also feared being pushed out of orientation too soon, putting their newly acquired licenses in jeopardy. They verbalized feelings of helplessness, isolation and the lack of supportive and nurturing relationships with management team and coworkers. In addition, some expressed dissatisfaction with lower starting salaries than other local hospitals. Grady nurse leaders used this information to direct their efforts of retention.
Collaborative Teamwork
Once the retention became the common goal, Grady was able to move forward to improve outcomes. Changes made by the stakeholders incorporated the concepts and actions deemed important to millennials: technologically based communication, minimal response time, timely information, clear direction, safe and social work environments, relationships with peers and mutual respect. This included efforts to recognize them for their accomplishments.
Human Resources
This department hired a senior talent acquisition specialist primarily assigned to recruiting graduate nurses. This person is responsible for the oversight of the nurse resident candidate including timely and efficient communication, processing applications, selecting interviewees, the interview process, hiring and initial onboarding. Open and continuous communication with the nurse residency program manager allows for alignment of all nurse resident start dates. The contract/agreement is discussed and presented prior to hire. The department developed qualification criteria for residents seeking specialty units. Residents have the option to choose up to three areas of interest for interview. The team now requires mandatory attendance of the program manager/unit management team during interview events. The shared governance council members interact with nurse residents and share experiences while the residents are awaiting interview appointments.
Department of Nursing Education, Practice and Research
The director of this department eliminated the program coordinator assignment and replaced that position with a program manager. A facilitator was assigned to assist with the program. This department now has overall responsibility for maintaining retention data and supporting the needs of the nurse residents. The department creates strategies and communicates with leadership about the needs of the program. It provides consultative services and guidance to the program manager. In addition, the department provides guidance, escalates concerns, evaluates the program and assures that the ACNE/CNE prioritize the nurse resident.
Unit Management
Unit managers assure nurse residents are welcomed and positively supported throughout orientation and the first year. They adhere to and support the nurse residency program curriculum and activities. They assure preceptors have received education and/or attend workshops and assign committed preceptors. Unit managers are now highly encouraged by the nursing executive team to attend nurse resident presentations/graduations, communicate and collaborate with program manager concerns and challenges.
Program Coordinator
The program coordinator manages all aspects of the nurse resident for first 14 weeks of orientation or when the nurse resident meets baseline competencies to provide safe patient care, fully supporting the nurse resident journey. She or he advocates, counsels, supports and communicates the residents’ individual or group needs/concerns, has strong collaboration with human resources, the unit management team, and ACNE/CNS. He or she also holds educational in-services for the leadership team on the residency program and created “Guidelines for Leadership” providing detailed information about the program and stakeholder expectations and responsibilities.
Advanced Clinical Nurse Educators
ACNEs meet with nurse residents initially and weekly during orientation, supporting their needs during the first year. They are responsible for all phases of orientation and monitor preceptor and nurse resident relationships, providing education and guidance to preceptors. They develop professional relationships and trust with the nurse resident and act as a liaison for the nurse resident in various situations. ACNEs guide nurse residents’ evidence-based projects and also communicate and work closely with the program manager.
The changes made by the stakeholders in the past two and a half years have directly impacted the retention of the nurse resident at Grady Health System (Table 1). The nurse resident is a priority of the organization at all levels. The experience of horizontal hostility is significantly reduced; preceptors are taking an interest in the nurse residents’ success. Nurse residents are developing relationships with their preceptors, staff and management team and say directors are more visible and engaged in their well-being. Executive leadership personally addresses the nurse resident concerns by attending sessions, encouraging and accepting open honest dialogue. Nurse residents now receive a significant monetary boost to their salary upon completion of the program, a true concern of millennials. Opportunities are provided to build collaborative relationships with health care members in various departments who impact their ability to do their jobs effectively through hospital rotations. Grady supports their need to explore career opportunities by arranging shadowing experiences for those looking to transfer to other clinical units after their first year. Preceptors are required to be trained and receptive to the nurse resident. The program manager remains their primary advocate so that they are heard and positive outcomes are realized.
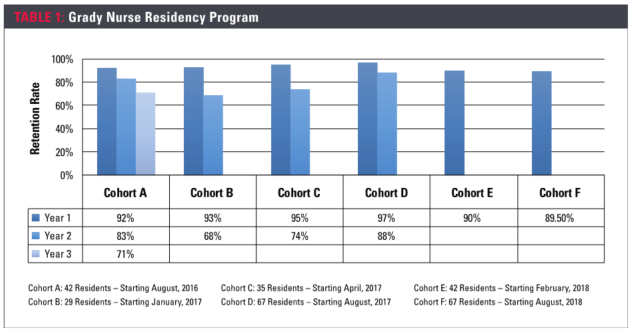
Grady leaders have learned retaining the nurse resident during the first year is a collaborative effort requiring executive leadership support. A common goal enabled the system to drive necessary processes forward to maintain a culture supportive of new nurses. Overall, nurse resident feedback has positively improved and the first-year nurse resident average retention rate has been 93–95% since 2017.
“It takes a village” is an old African proverb meaning that a child’s upbringing is a communal
About the Author
Deborah R. Davis, MSN, RN
Clinical program manager nurse residency program, Grady Health System, Atlanta.


