
Hot Topics | Care Innovation
Using a COVID-19 RN Advice Line
In early February 2020, U.S. health care systems watched with growing concern as COVID-19 reached the nation, affecting states, local communities and the entire health care infrastructure. Nationally, the number of patients with COVID-19 symptoms, confirmed exposures and potential exposures dramatically increased between February and early March 2020 (Omer, S. B., Malani, P., and Del Rio, C., 2020). Urgent and emergency care services swelled as anxious patients overwhelmed hospital and medical office phone lines, seeking information and reassurance. In order to manage the public’s mounting fears and anxieties around COVID-19, Sutter Health developed a solution—an RN advice line —in five business days.
Sutter Health, based in Sacramento, an integrated network of clinicians, employees and volunteers, provides care to more than 3.5 million northern Californians. With the number of COVID-19 cases rising, Sutter leaders recognized the need to mobilize a workforce that could triage an unknown number of patients experiencing symptoms to the right level of care quickly. The COVID-19 RN advice line was Sutter’s first line of intervention for patients worried about COVID-19.
COVID-19 protocols were rapidly developed; advice line training was created and recently displaced RNs were recruited to staff it. This telephone-based advice line was made available to surrounding communities, allowing potential victims of this emerging disaster to receive information and seek treatment.
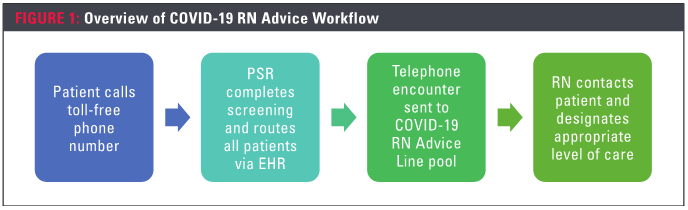
The RNs used a script to set expectations for the type of advice they would deliver and then utilized a workflow differentiating between asymptomatic and symptomatic patients. The RNs assessed patients, determining if symptomatic patients should call for emergency transportation, go to a local emergency room or urgent care, or treat themselves at home. Education was developed to guide patients on how to self-quarantine and use appropriate protection when away from home including using face masks, washing hands and social distancing. For asymptomatic patients with questions about the disease, the advice line provided accurate and useful information using published CDC patient education.
Leveraging the HER
To align with California state RN scope of practice, Sutter adapted an existing nursing standardized procedure (SP) for telephone triage. RNs giving medical advice are required to create and be competent using a SP. Required elements for this SP document include initial competence and annual training. Using subject matter experts, the steering committee developed key phrases for documentation that met the state SP requirements.
These key phrases allowed the RNs to quickly document COVID-19 advice calls. For example, screening phrases were used for each call to consistently document exposure, symptoms, previous care, risk level, vital signs at home, patient education and disposition determination.
The patients were given instructions via the patient medical record portal including home care instructions, emergency warning signs and tips for caregivers. RNs educated the patients about symptoms and COVID-19 safety precautions.
Utilizing a virtual phone line installed on a company laptop, RNs used an existing phone system platform to facilitate incoming and outbound patient calls. The software provided real-time information on the type of patient call, where the patient was in the queue and number of PSRs and RNs available. This allowed supervisors and clinical leads to monitor real-time performance, view metrics and provide feedback to improve the use of protocols and workflows, as well as monitor patient interactions and queue statistics. For patients requesting additional languages, a dedicated interpreter service was available to assist RNs.
Training
Telephone triage was not familiar to the RNs, and some had to learn various EHR features, notes Cathy Leon, RN, director of clinical practice, education and development. “This was a scary time for them, but they quickly learned,” she said.
Specific COVID-19 training and resources were created and posted electronically to an internal learning hub. Documents were updated in real time as guidelines changed for patient education and management. Additional RN training was provided to support knowledge gaps identified in team calls. Because the RNs had varying levels of experience, documentation training was provided at both beginning and advanced levels.
“Training was simple and straightforward,“ said triage nurse Jules Crawford-Grover, RN, adding that internal learning page explained the workflow, but allowed RNs to apply their clinical knowledge within the boundaries of the SP.
Opening the lines
On March 11, just five days after creating the COVID-19 advice line team, Sutter opened the phone lines, serving a geographic area covering 15,192 square miles. Six days later, on March 17, the second COVID-19 advice line went live, covering another 8,871 square miles.
“During the first two weeks, [many of the callers] thought they were dying. Education was the most helpful thing for patients; they weren’t sure if they had [COVID-19],” said Crawford-Grover. “Our patient population had been really scared and it was nice to provide education on symptoms and what to watch for. Some patients were very sick and needed to be seen right away. If a patient is struggling to breathe, being able to quickly get them to the right level of care is critical.”
Advice line nurse Grace Chow, RN, added, “There were a lot of calls where the patient said at the end [of the call], ‘I was anxious, but now I feel better with the information you gave me. I’m going to do these steps for home care.’ The patients were happy to know they were taken care of and that we were watching out for them.”
Expanding coverage
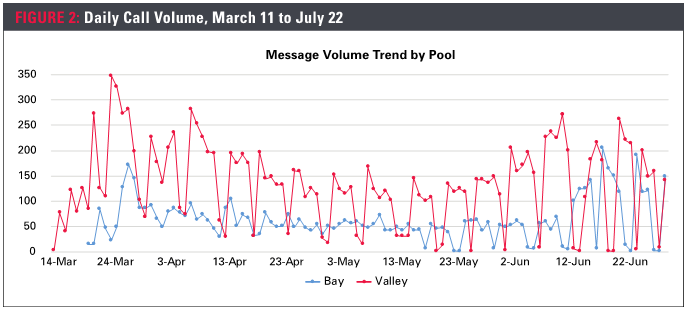
Within three weeks of opening the COVID-19 RN advice line, patient volume increased dramatically. On March 11, the advice line went live for Sutter Health Valley area (phase one) and on March 17, for Sutter Health Bay area (phase two). March 23 and 24 saw the largest volume at 474 and 498 daily calls (Figure 2).
Initially, the COVID-19 advice line was intended only for Sutter Health’s established patients. “News channels posted our number prior to us providing non-patient access—the number got out there before we were ready,” said Ana Wilden, advice line project manager. “People who had never been seen at Sutter Health were asking us for information because they knew we were providing accurate advice. Sutter Health is a trusted source in the community.”
Recognizing a larger need, Sutter extended the COVID-19 RN advice line to all community members on April 1 and planned for an increase in call volume. Patients calling from neighboring areas were directed to their local urgent and emergency care providers, Wilden said. A social media campaign was launched to promote the COVID-19 advice line to the broader community. By May 26, 2020, just under 2,000 non-Sutter patients had utilized the line. Once the initial RN staffing was complete, additional RNs were brought in four more waves to accommodate volume. Calls were covered for a total of 12 hours per day, seven days per week.
Chatting to provide support
The RNs working the COVID-19 advice line were from many different departments, affiliates and geographic areas and most had never worked together. Using the secured chat function of virtual meeting software, RNs were able to message questions to the entire group in real time. Both peer RNs, supervisors and clinical nurse educators responded to the messages, often as quickly as one minute.
A wide variety of topics were discussed internally on the chat, including patients calling about the risk of chronic diseases like diabetes and COVID-19 infection, testing following exposure to a confirmed COVID-19 patient and where testing was available in their communities. Having the interactions documented in a chat format allowed for all RNs to access the questions and answers. After seeing questions asked multiple times, the clinical education leads developed a frequently asked questions document to place in the resource section of the shared site.
Chow said the chat function was a uniting force. “I started to build a bond with the other clinical support RNs and we were helping each other even when we were not working the advice line.”
“Watching the COVID advice line nurses chat has been so inspiring,” said Leon. “The RNs throughout Sutter coming together to provide patient advice and support to one another has been one of the best examples of nursing collaboration that I have ever seen.”
Call results
On March 11, 2020, Sutter took the first patient call. Eleven weeks later, the COVID-19 RN advice line had assisted more than 13,000 patients with COVID-related questions and symptoms and provided support to operations during this unprecedented pandemic.
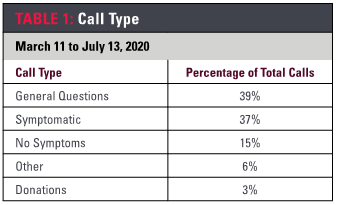
The largest portion of calls (39%) were from patients asking general questions about COVID-19 (Table 1), followed by patients who were determined to be symptomatic (37%). Symptomatic patients were triaged to an advanced practice clinician for testing discussions or to urgent or emergency care. Only 15% of patients who called the COVID-19 RN advice line did not have any symptoms.
As a not-for-profit health care system, Sutter was appreciative to receive donations from approximately 3% of the COVID-19 RN advice line calls. Donations ranged from cash to medical supplies.
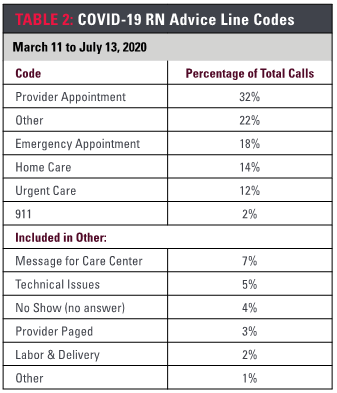
Upon completion of each call, the advice line nurses used codes to categorize the triage decisions (Table 2). One-third resulted in appointments with primary care providers, one-third resulted in urgent or emergency care. The remaining third comprised a combination of home care advice (14%) and messages for follow-up (“care center”, 7%; “provider paged”, 3 %”) as well as a mix of issues not related to direct patient care.
On-demand advice line workforce
In early June, call volume slowly decreased to less than 300 calls per day and ambulatory care sites began to reopen. RNs were being pulled back to the surgery centers and other procedure areas so the Salt Lake City advice center began to manage the calls. Sutter continued to closely monitor local rates of infection and created a plan to reengage the COVID -19 RN advice line RNs if the call volume surged.
The advice line nurses are prepared to help again when needed, thus creating an on-demand team that can be deployed should the volume begin to climb. The COVID-19 RN advice line steering committee agreed that a spike of calls would trigger a notification for needed advice line staff. Additionally, the advice line nurses unanimously supported participation in brief monthly training to keep their COVID-19 advice skills current.
“We will have nurses trained and ready to activate during a surge,” said Wilden. “We can put out word that the call volume is too high, and nurses are needed to support the line. Nurses have told us they are happy to do it because they can apply critical, timely clinical decision-making. They enjoy the calls because they are truly working at the top of their license.”
COVID-19 RN advice line nurses retained access to call pools and some continued to take calls, when available. Back at work in an allergy clinic, Crawford-Grover noted, “I’m already logged into my computer during the day, so I log in as needed and take calls when I’m in between patients in clinic.”
Sutter plans to maintain the COVID-19 RN advice line for as long as necessary and is evaluating expanding the use of standardized triage software across the system. This communication model could be applied to future scenarios. “The innovative COVID-19 RN advice line allowed us to connect with patients one-on-one to deliver safe, personalized, high-quality care in our local communities, said Sutter Health Chief Nursing Executive, Anna J. Kiger, DNP, RN. “Our advice line nurses continue to be a compassionate and steady force for patients and their families during COVID-19.”
Reference
Omer, S. B., Malani, P., & Del Rio, C. (2020, April 6). JAMA. The COVID-19 pandemic in the US: A clinical update. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2764366
About the Authors
Surani Hayre-Kwan, DNP, MBA, FNP, FAANP, is director, professional practice and nursing excellence
Anna Kiger, DNP, RN, NEA-BC, FAONL, is chief nursing executive
Julie Snoke is an advanced practice clinician program manager


