
Inclusive Nursing Leadership: Training to Address Racism
In this time of nursing shortages across the nation, organizations need to be able to recruit and retain nurses and particularly nurses from diverse backgrounds. Seattle Children’s Hospital (SCH) is committed to creating a workforce that represents the patients it serves, and having an organizational focus on equity, diversity, inclusion (DEI) and antiracism as evidenced by the strategic goals and initiatives in SCH’s Health Equity and Antiracism Plan. Parallel to this work, SCH leaders developed a nursing strategic plan with the goals of increasing and retaining a racially and ethnically diverse nursing workforce, while also improving health equity of our patients and families. Many nurses want to work for an organization inclusive of diverse backgrounds and perspectives, thereby creating a bridge to understanding the experiences of their diverse patients. It is also important to recognize that the inclusivity of the work environment, leader support provided for staff and the trust between leadership and front-line staff can affect recruitment and retention as well.
HEAL Council creation
One project within the nursing strategic plan was the creation of a nursing shared governance council related to health equity, diversity, inclusion and antiracism named the Health Equity through Activism and Learning (HEAL) Council. The HEAL council is comprised of staff nurses representing units and departments from across the organization. At its inception, the council conducted a survey in early 2021 with more than 400 respondents, including 72 nurse leaders. The survey’s aim was to understand the experiences nurses had with racism at SCH.
The survey results highlighted several gaps in meeting the organizational goals of inclusion and anti-racism, particularly in the front-line staff perception of nursing leadership’s ability to address issues related to equity, diversity, inclusion and anti-racism. This includes situations when staff experiences racist attitudes from patients and families, and when patients and families experience racism from staff. Staff were not confident that leaders were modeling behaviors promoting an inclusive environment and demonstrating the leaders’ commitment to organizational goals (Figure 1). The survey results also highlighted a lack of resources, skills and knowledge in how to approach these issues. Nurse leaders often have situations escalated to them by both families and staff, and are called upon to find resolutions and to provide feedback and coaching.
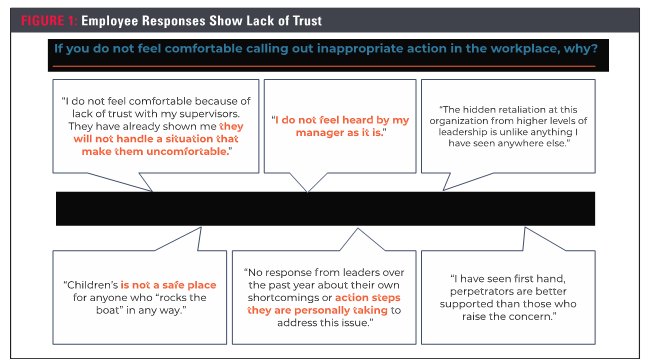
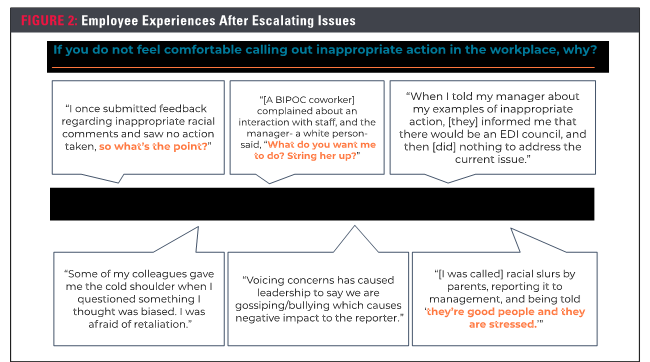
At times, nurse leaders are called to be mediators during conflicts between staff in which a subtle comment or action expresses a biased attitude toward another staff member. These are called microaggressions, and are directed toward a member of a marginalized group, often unconsciously or unintentionally. SCH nurse leaders conversely have reported a lack of confidence, knowledge and skills in addressing racial tensions among staff. In addition, nursing staff have reported being fearful to speak up when issues of race are present, and have expressed concern for retaliation from leaders or peers (Figure 2). The project goal was to develop a more inclusive environment by teaching nurse leaders skills for dealing with microaggressions among their staff. Trust between staff and leadership and a rapport encouraging staff to engage in DEI work fosters an assurance that leadership is actively listening to and supporting the voices of racially and ethnically diverse staff.
Responding to microaggressions
In order to address these issues, representatives from the strategic planning group were able to connect with a local organization to provide relevant, effective training for nurse leaders. The training provided a mental framework on listening to understand the perspectives of staff members when tension exists, being genuinely curious about those perspectives and ways to approach mediation and resolution when microaggressions and acts of racism occur. The training took place on Aug. 30, 2022. Prior to the training, organizers conducted a survey of nursing leaders to evaluate their preparedness for conversations with their staff to understand the potential impact of this training. The training included discussion on coaching on impact versus intent, evaluating the group’s experience with microaggressions, engaging staff in non-verbal communication and how to coach when cultures clash. Resources provided during the training can be applicable to various conversations conducted with staff members.
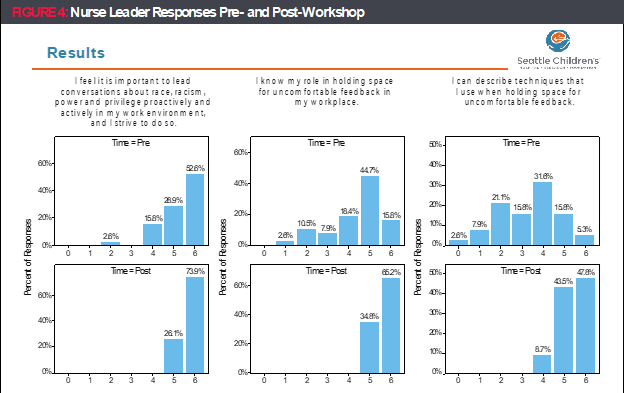
Forty-two nurse leaders participated in the workshop, with 38 (90.5%) completing the pre-survey and 23 (53.8%) completing the post-survey. The survey findings overall showed statistically significant improvements in the responses for nine out of the 10 survey questions, obtained on a 7-point Likert scale. Nurse leaders reported significant improvements in their skills and ability to address microaggressions, have courageous conversations and have opportunities for uncomfortable feedback (Figures 3 and 4). One of the survey questions asked leaders about their overall level of comfort and confidence in all of these areas. In the pre-survey, just 10.5% reported they were “moderately comfortable” overall, whereas in the post-survey, nearly 61% of nurse leaders reported this same level of comfort. Another question asked if leaders could “describe techniques for facilitating courageous conversations, in both small and large groups.” In the pre-survey, no nurse leaders moderately or strongly agreed with that statement, while in the post survey, 69.5% moderately or strongly agreed.
The responses and comments from participants after the workshop demonstrated high value for these participants in their paths to be inclusive nurse leaders, particularly in the role-play and skill-building portions. This project contributed to furthering the organization’s strategic imperative to become an anti-racism organization and build a diverse and inclusive culture. There is a lack of guidance in nursing literature on how to address these issues in practical ways. More investigation into best practices leading to measurable outcomes is needed as part of the effort to tie inclusive nurse leadership to the provision of equitable care.
Looking forward
It is vital for nursing leaders to be responsive to the needs and concerns of their staff and patients when it comes to issues of microaggressions and acts of racism. By providing resources and training to nurse leaders to be able to respond to these issues, the trust between leaders and staff can be strengthened. In addition, leaders are better able to provide the supportive and inclusive environment staff will want to work in. The results of the SCH survey produced revealing information, demonstrating the impact of staff experiences with racism and in turn, their concerns about informing their leaders about these instances. Within the power dynamic between staff member and leader, the goal is to create an environment that is less intimidating for staff and diminish any concerns of retribution or mistreatment. The overall desired outcome of this work is iterative and demands the engagement and intentional effort to learn and commit to change by the nurse leader. Within this pilot, the commitment of the participating leaders was clear. SCH continues to offer these workshops so nurse leaders will feel comfortable addressing situations when they are escalated. This in turn will create a better environment for nurses and patients alike.
ABOUT THE AUTHORS

J. Mari Moore, MSN, RN, NPD-BC, is a nursing professional development practitioner working on equity, diversity and inclusion initiatives at Seattle Children’s Hospital.

Christina Finch, MHA, BSN, RN, CPN, is nursing director of an inpatient medical unit at Seattle Children’s Hospital. She assisted with this initiative as part her work to complete the AONL Nurse Manager Fellowship.

Juliette Ofamen, BSN, RN, is a nurse in the post-anesthesia recovery unit at Seattle Children’s Hospital.

